
Medical mysteries -- can you solve them?
King George III was famous for having episodes of poor mental health. His exact diagnosis is still debated but what did a strand of his hair reveal?
Historians and Physicians have hotly debated King George’s health for many years. His erratic writings have been compared to the outbursts of patients with bipolar disorder. However, he also displayed symptoms similar to someone suffering from the genetic blood condition, Porphyria. This is where the body struggles to create haem, which makes haemoglobin, found in the red blood cells to carry oxygen around the body. Porphyria can lead to mental confusion, hence, the link made to his other psychological symptoms. In 2005 a strand of King George’s hair was analysed revealing high levels of the poison, arsenic. It’s likely that he consumed it through a medication he was given by doctors at the time called "James’ Powders". And so the medication he was given was probably making his condition worse rather than better (source).
Morgellons Disease is a condition that has been described as having ‘sci-fi like symptoms’. These include:
Morgellons Disease is a controversial condition which little is known about. Some doctors view it as a physical disorder of the skin whilst others associate it with a type of psychosis where patients have delusions that their skin is infested with parasites. Patients complain of red sores that appear suddenly and take a while to heal, very itchy skin, thread-like fibres that stick out of the skin, extreme tiredness, joint pain and difficulty sleeping. Research into this rare condition is ongoing (read more).
Pica is a disorder that gives a person a strong urge to…
Pica is an eating disorder that makes a patient want to eat non-food items like chalk, metal, paint, and ice, which do not offer any nutritional value. It’s not always clear why some people develop this condition. Iron-deficiency anaemia and malnutrition are two of the most common causes of pica, followed by pregnancy (source). It’s thought that in these cases, the body is trying to make up for something its lacking. Pica can also occur as part of a mental health issue such as Autism or Schizophrenia (source).
What is meant by a 'congenital' disease?
'Congenital' means ‘present from birth’ and can include genetic disorders such as Down’s Syndrome, cleft lip, congenital heart disease and Spina Bifida. Sometimes this may be passed on by a parent’s genes, sometimes environmental factors play a part (e.g. exposure to certain chemicals, infections, drugs/alcohol, and restricted access to a nutritious diet) and in other cases, there is no clear reason why a child is born with a particular condition. There are several different tests available to expectant mothers (such as ultrasound scans, blood tests etc.) which can indicate whether a baby has a congenital disorder but sometimes it is not known until a child is born (source). Progress is happening relatively quickly though. Remarkably, with Spina Bifida, new advances in medical technology are allowing doctors to operate whilst babies are still in the womb (source)!
How many people in the UK will be affected by a rare disease at some point in their life?
This may sound like a lot but there are between 6000-8000 different types of rare diseases. The European Union defines a rare disease as one that affects less than 5 in 10,000 of the general population (source). In the UK, a single rare disease may affect up to 30,000 people but in reality, many affect far fewer than this (source). With some only affecting a handful of people or even just one single person in the whole of the UK (the ONS estimates that there are ~67.59 million people in the UK in 2022).
The Plague hit Europe and Asia in the mid-1300s wiping out more than 20 million people in Europe alone. But what did medieval doctors put the spread of the disease down to?
Medieval doctors did not have the kinds of tools and medical knowledge we might take for granted today e.g. that germs exist and we can combat them with good hygiene habits. Some of their treatments would be considered bizarre by modern-day standards e.g. rubbing onion, herbs or dead pigeon into wounds or drinking vinegar (source)! However, others were pretty sensible, for example, it was the first time that quarantines were used (whereby infected patients were isolated from the wider community). And although they didn't understand which ones, they also recognised that animals could be carriers of the infection and tried to cull cats and dogs as a means of reducing transmission. It didn't work but the thinking was there. It wasn’t until the 19th century that scientists discovered that the plague could be transferred to humans via the bite of an infected rat flea!
What is it about zebrafish that’s helping researchers to learn more about heart disease?
Similar to how our bodies can mend a broken bone, zebrafish can repair damaged heart tissue in a matter of weeks. Researchers at Oxford and Sheffield Universities are trying to understand how this amazing process works to see if we can learn new ways to treat patients who are experiencing heart failure. Zebrafish are transparent in early life making it easy for researchers to see their growing organs. Scientists are then able to inject the fish’s cells with different coloured dyes to see how their hearts grow. They can also turn off genes and see how the zebrafish regrows blood vessels to repair damage. It’s hoped that research like this can help medics support patients who’ve had a heart attack - enabling them to live longer, healthier lives. Watch more.
True or false: It's universally understood that a disease is when someone has physical signs that their body is not working as it should.
It’s true that a disease is a condition that prevents the body or a particular part of it from functioning normally and which produces specific symptoms. But this can include emotional and psychological symptoms in addition to physical signs of illness. Definitions of disease have changed over time and vary among different cultures. A lot depends on what you define as ‘being healthy’ in the first place (read more).
What are ‘Superbugs’?
Superbugs are types of bacteria that no longer respond to certain antibiotics (source). Bacteria naturally evolves over time, however particular factors have accelerated this process to the extent that medical advances are struggling to keep up. These factors include: the overuse and misuse of antibiotics, poor infection control, inadequate sanitary conditions and inappropriate food-handling. This could have serious implications especially for patients recovering from surgery, and undergoing treatments such as chemotherapy (source).
Vive la vaccination!
Have you ever had a vaccination injection at the doctor’s office or at school? Then you’ve probably heard about the basics – how the injection helps ‘train’ your immune system by presenting it with a weakened version of an illness so that it’s ready to fight the real thing.
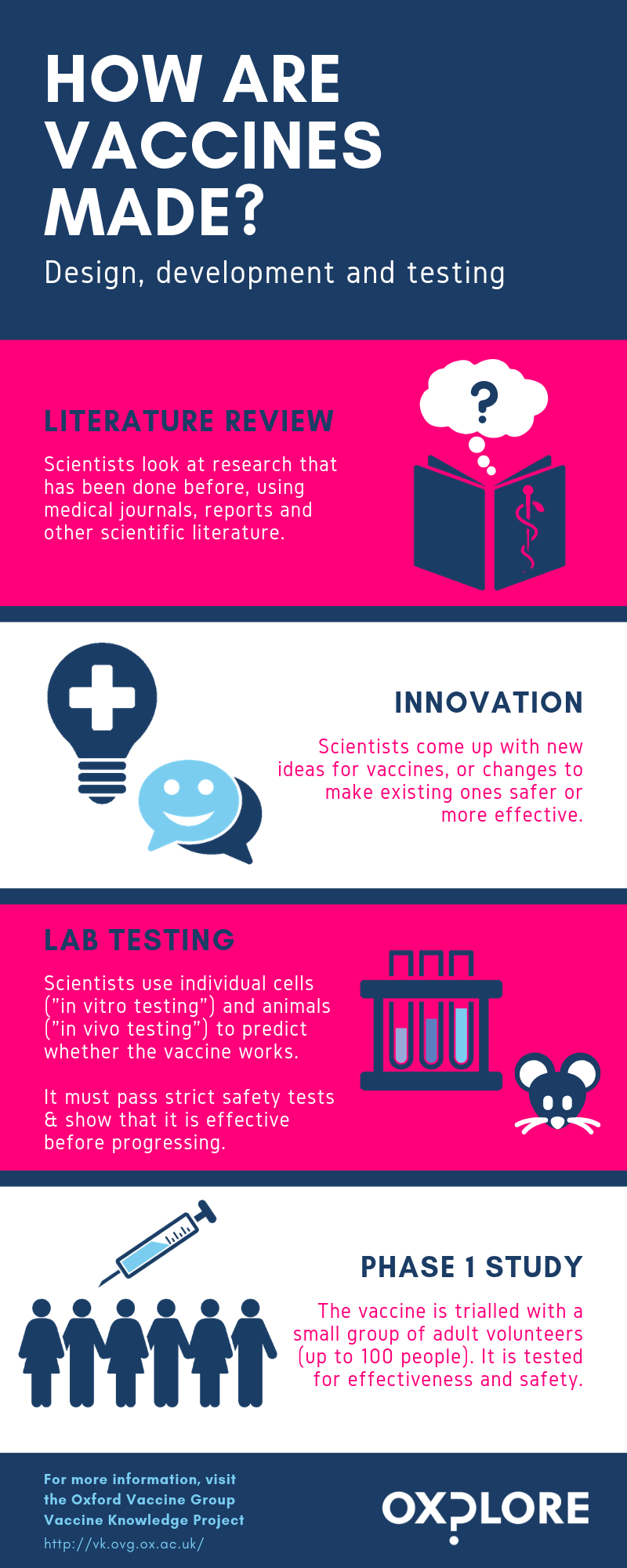
How are vaccines made and tested?
Understandably, people are often concerned to know how well vaccines have been tested before they are used on human beings. In the UK, the standard for testing and monitoring of vaccines is higher than it is for most other medicines, because they are one of the few medical treatments given to healthy people (mainly healthy children). This means that the level of acceptable risk is much lower than it might be for a cancer treatment, for example.
This graphic shows all the stages that a new vaccine needs to pass through before it can be given to people. It can take many years for a vaccine to pass through all the stages – for example, in the case of the MenB vaccine for meningitis (a dangerous bacterial infection which attacks the brain, blood and spinal cord), it took nearly 20 years from the first idea to the vaccine being licensed for use.
What impact has the invention of vaccination had on diseases?
Case study: Smallpox
Smallpox was a viral disease caused by the variola virus. It caused an illness which had lots of different symptoms – including making people develop a rash of pustules (large, painful fluid-filled sores) covering their entire body. On average, it took the rash 24 hours to cover the body and an additional three weeks for pustules to grow in size, form crusts and eventually fall off. The rate of death for the more common and dangerous variola major strain of the virus was estimated to be around 30%. People who survived would often be marked for life with scarring from the pustules, which could be very severe.
Smallpox had been around since at least the time of the Ancient Egyptians, and there was no successful treatment other than letting the disease run its course. However, some groups of people in China and India practiced variolation – a technique of introducing people, especially young children, to the smallpox virus in the form of liquid from the pustules of ill people or dried pustule scabs which were inhaled in controlled quantities. This usually caused the person to develop a milder form of the disease, which then gave them immunity (although sometimes they unfortunately caught the full-blown version and died). At the end of the 18th century, the British doctor Edward Jenner extended this technique to pioneer the first ever true vaccination, using the related cowpox virus to protect patients. His discovery was based in part on information about variolation that Lady Mary Montague, the wife of a British ambassador, had sent back from Istanbul in the 1710s (Read more).
Tip: Jenner invented the smallpox vaccination in 1796 -- using a calculator, find the average share of smallpox deaths in the ten years before this (1786-1796) and the ten years after (1797-1807). Then compare these to the ten years after that (1808-1818). What happens over time?
Footnote: Note the big jump in smallpox deaths in 1871 – this is an anomaly linked to the Franco-Prussian War of 1870, when transporting French prisoners of war who hadn't been vaccinated contributed to a smallpox epidemic which killed more than 500,000 people across Europe (Source).
Be aware that this data comes from a time when other standards, like cleanliness and access to trained health care workers, were also on the rise, so these factors might be playing a role too!
Following World War II, the World Health Organisation declared a resolution to eradicate smallpox around the world and launched its Intensified Smallpox Eradication Programme in 1967. The last known case ‘in the wild’ was reported in Somalia in 1977. Since then, scientists estimate that this has saved around 5 million people’s lives per year.
So why would people not want to be vaccinated?
Given all this, why would some people not want themselves or their children to be vaccinated? One relatively recent reason is a piece of discredited research published in the 1990s by former physician Andrew Wakefield, linking the MMR (Measles, Mumps and Rubella) vaccine with autism. Although this research was found to be based on false data and retracted by the medical journal which published it (and Wakefield has since been barred from practising medicine) the idea had taken hold in many people’s minds. At around this time many people also became concerned about the ethics of the big pharmaceutical companies manufacturing the vaccines, and about whether they were allowing their business interests to override their duty to protect people’s wellbeing.
A 95% immunisation rate is required to maintain herd protection, but after Wakefield’s ‘research’ was published immunisation rates dipped below 80% in the UK, and measles infections rose (source).
The UK immunisation rate for MMR is now back up over 90%, but it has been dropping over the past five years (2015-2019), and the UK recently lost its World Health Organisation status as a "measles-free" country (source).
Do you have to be a doctor to cure diseases?
-
Currently, medication tends to be given to patients via a pill or injection that then enters their blood stream and attacks the disease or infection in question. The downside of this is that all cells - even healthy ones - are exposed to this treatment. In the case of the cancer treatment, chemotherapy, this over-exposure can make the patient have unpleasant side-effects and feel very unwell. Biomedical Engineer Prof. Eleanor Stride is leading research into injecting tiny microbubbles of medication into a patient’s bloodstream. This allows the treatment to be more targeted as the drugs are only released once they reach the part of the body that needs it, e.g. at the site of a cancerous tumour. Some of the bubbles are magnetic which means that they can be dragged to a specific location using a magnet from outside the body. The team then use ultrasound technology to vibrate the bubbles, releasing the drug and “pumping” it into the tumour to maximise the number of cancer cells that are exposed.
-
Imagine a drug that can diagnose and treat an illness... It might be that the active component of the drug is concealed in a capsule that is targeted to a specific site in the body. Perhaps the capsule will only open and release the drug after a diagnostic test has been run. This kind of smart drug would only act when and where it was needed. The DNA group at Oxford Physics hope to be able to design smart drugs in the future. For the time being, they are working on capsules, the mechanisms for opening them and simple devices that perform tests -- for example, devices that test for the presence or absence of a molecule. This work uses DNA as a building material. In fact, a carefully designed set of DNA strands are heated and gradually cooled down and they then assemble themselves into a pre-planned structure. Select molecules, for example a protein, can then be loaded into this capsule and access to this cargo can be controlled by opening and closing the capsule. Although there are many challenges remaining, this work, and similar work done in research groups across the world is a step towards drugs that treat diseases more effectively (not at the expense of healthy cells) and treatments that can be personalised according to the unique needs of a patient.
-
- Much of life on Earth is made up of large, repeated molecule chains called polymers. The top three are: collagen (found in our bodies), cellulose (found in plants) and chitosan (found in the shells of crabs, shrimps and other crustaceans). Prof. Sonia Contera (Department of Physics) is leading research with Dr Alex Gordon-Weeks (Nuffield Department of Surgical Science) into how physics can improve our understanding of pancreatic tumours and eventually make treatments more effective. This involves using a particular type of microscope (an Atomic Force Microscope) to look at how collagen functions within a pancreatic tumour and specifically, how it controls the movement of molecules. Currently, chemotherapy has limited success in treating patients with pancreatic cancer. This is thought to be due to the structural characteristics of pancreatic tumours (e.g. the stiffness of the collagen mesh that forms their structure), which may prevent drugs from being able to flow within the tissue. And so a better understanding is needed... this is where drawing upon the general laws of physics comes in, together with the use of the Atomic Force Microscope. This is because it is the only tool that can produce images of biological systems in fluid at a very tiny scale. More than this, it uses a tiny tip to apply force to a sample, which can determine its mechanical properties such as the stiffness of the material or the flow of fluid within it. This information will be used to improve detection and treatment of cancer.
-
As the name suggests, Magnetic Resonance Imaging (MRI) relies upon the power of magnets to scan and assess different parts of the body - magnets so strong they could pick up a small truck! MRI scanning works by causing the hydrogen in water molecules in the body to spin around. As the protons in hydrogen are like little magnets it means we can use radio waves and antennas to get information about the water and the environment it is in (i.e. the patient). Find a more detailed definition here. Biomedical Engineer, Prof. Daniel Bulte conducts research into the way that MRI scanners can be used to track the flow of oxygenated blood as it travels to and around the brain when it performs different functions, and how it behaves in healthy and diseased tissue. In particular, he is interested in how the blood vessels in the brain open and close to control the supply of blood and how this system can fail in diseases like dementia and stroke. To learn more about MRI technology and its exciting possibilities, watch the video below: https://www.youtube.com/watch?v=wfi8CVCd8hw
-
Sometimes, the only way a patient with heart problems can access a better quality of life is to have a replacement heart valve fitted. Mechanical valves (created from man-made materials) are strong and durable but patients often need to take medication throughout their life to reduce the risk of blood clotting. Meanwhile, a patient fitted with a tissue valve replacement (treated pig valves) won’t usually need to take any medication but will likely need further surgery since these types of valves are not as long-lasting. And so, Sonia Iftekhar and her colleagues in the Oxford Biomaterials group are currently developing scaffolds (structures that provide temporary support for cells) that copy the way tissue in the heart valves work. Specifically, the team use natural materials to create scaffolds consisting of three distinct layers: a strong layer of collagen, a stretchy layer of elastin and a shock-absorbing layer of glycosaminoglycans. Each layer is made individually as a slurry (a semi-liquid mixture) and combined together to create tri-layered scaffolds. They then undergo a process called freeze-drying to give them a mesh-like structure. Heart cells are added on to the scaffolds and tested to see how they grow and produce new tissue. The team study the microstructure and mechanical properties of the engineered tissue to understand which factors promote healthy tissue growth and mimic the heart valve most closely. It’s hoped that one day this research will enable replacement valves to be personalised by using a patient’s own cells to create a heart valve that is both durable and biologically specific to them.

What about mental health?
Today, the NHS includes issues such as anxiety, eating disorders, ADHD and phobias under the heading of “mental health”, alongside psychiatric conditions like schizophrenia and bipolar disorder (source). But this wasn’t always the case - how did people in the past think about mental health and mental illness? How do we understand mental health today, and how could that change in the future?
A short history of mental health
In the past, people thought about mental illness in a variety of different ways. These might vary according to people’s cultures and the places in which they were living – for example, at some points in European history people might have associated the symptoms of some psychiatric illnesses with witchcraft or the idea of being possessed by demons, and unfortunately sometimes those affected were persecuted or even killed.
At the court of Sultan An-Nasir Salah ad-Din Yusuf ibn Ayyub in Cairo during the 1100s some people thought ‘madness’ had something to do with possession by spirits, but they also believed that it could be caused by an imbalance of ‘humours’ or elements in the body. Some doctors also seem to have had a rudimentary understanding of the idea of depression, which they called ‘melancholy’. Muslim, Jewish and Christian doctors working at the Sultan’s court believed that people who were suffering from ‘melancholy’ needed pleasant company, music and the opportunity to engage with things they found interesting. They created herbal treatments and suggested activities such as reading good books on philosophy and religion to help. Learn more in this lecture by Daniel Nicolae.
The image above was painted into a book around 1185, and may be a portrait of Sultan An-Nasir Salah ad-Din Yusuf ibn Ayyub. Credit: Public domain.
In London during the 1600s and 1700s, people with serious mental illnesses were often locked up against their will in Bethlem Royal Hospital.
This had been built as a very luxurious and modern hospital for people who were too ill to take care of themselves - but it quickly went downhill as the building became run-down and the hospital began to raise extra money by allowing visitors to tour the hospital in order to look at the patients, and even laugh at them and taunt them. The name “Bethlem” became shortened to “Bedlam”, and due to the poor conditions in which the patients lived “Bedlam” eventually became a synonym for any place or situation that was disordered, noisy and chaotic. Read more.
The image below shows a patient, James Norris (sometimes known as William Norris), being held in restraints at “Bedlam” during the early 1800s. Images like this led people to campaign for better conditions for the patients. Credit: William Norris, shackled on his bed at Bedlam: Wellcome Collection.
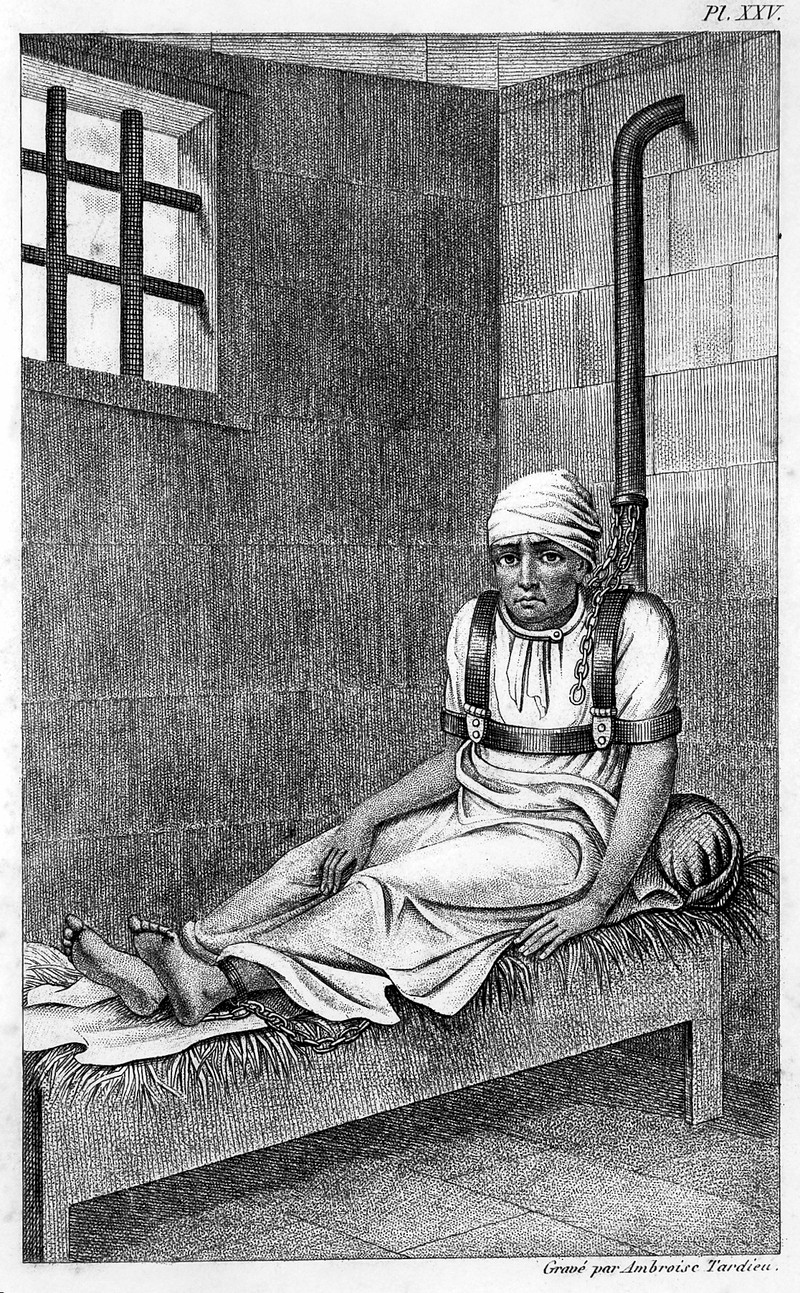
What do you think? Did “Bedlam” make life better for people with serious mental illnesses, or did it make their lives worse? Consider that the alternatives to being confined to hospital may have been living on the street with no access to food or shelter.
During the Victorian period, people started to think a bit differently about mental health. Two new inventions - the railway and the ‘penny post’ which allowed people to send each other letters quickly and often - made many people feel that the pace of life was ‘speeding up’. They suddenly had to cope with lots of new information arriving in the post (some people got up to 12 mail deliveries a day!) and the ability to travel to different towns and cities very quickly. Many people worried about the impact of these stresses on their “nerves”, by which they meant their ability to cope with everyday situations and anxiety.
This might sound a bit familiar - people nowadays often report feeling similarly bombarded by emails and social media notifications or exhausted by aeroplane travel. The Diseases of Modern Life Project at Oxford University has spent the last few years studying images, documents and statistics from the past to learn more about how Victorian people understood the impact of stress on mental health.
How are things changing?
Nowadays, there is an increasing shift in the media to share people's mental health experiences and to create greater awareness of what support is available - helping to make those who are suffering from mental illness feel less isolated.
For example, the UK-based charity Comic Relief led a campaign in 2018 which involved a mix of celebrities and members of the general public sharing their experiences. The campaign suggested that mental illness can affect anyone at any stage of their life, and so we all need to take care of our mental health. The message that unites the speakers' experiences is the importance of talking to someone and not suffering in silence.
https://www.youtube.com/watch?v=tv82K_M7o5A
At the same time, more and more schools are considering how mindfulness training and activities can be included in the support they provide to students. Researchers at the University of Oxford have been leading studies into this very area via the MYRIAD project. The project is based on the knowledge that childhood and the teenage years are a vulnerable time for the start of mental illness: 75% of mental disorders begin before the age of 24, and half by age 15 (Kessler et al., 2005). The Department of Health (2011) recommends that “By promoting good mental health and intervening early… we can help to prevent mental illness from developing and mitigate [reduce] its effects when it does”. With this in mind, the MYRIAD team have taken an 8-week Mindfulness course which is known to be effective in preventing depression and promoting mental health in adults, and adapted it to work and appeal to teenagers in a (mainstream) classroom setting. For a definition of mindfulness, check out our article in our ‘Are we getting unhappier?’ big question.
The role of digital technology and mental health
Through her work on the Be-GOOD project, Prof. Ilina Singh (Department of Psychiatry) studies young people’s ethical and moral understandings of key issues related to mental health.
These include what it means to: experience personal agency (i.e. a sense of control over your choices); be a good citizen; lead a good life, and behave well. As part of this, the research team have focused on building digital tools to investigate young people’s moral and ethical attitudes to mental health innovations such as mental health apps. Another area of interest is young people's opinions on predictive technologies that could uncover the risk of mental ill health before symptoms have appeared.
Digital approaches to mental health service delivery could be seen as supporting young people in understanding their own mental health. On the other hand, these could be seen as over-generalising mental health challenges, or even encouraging young people to think they have a mental illness. This raises ethical tensions. For example, how should we balance the good that can come from better and more acceptable routes of access to mental health services for young people against the harms to personal identity and privacy that can accompany sharing deeply personal data on-line?

It also raises questions about what role a mental health app should play: should it replace or assist a doctor? Who is responsible for the ‘care’ offered and outcomes… Is it the app designers? The person who recommended the app in the first place? The app user? The technology itself? And how should new users be encouraged to join? Those suffering from mental health conditions may be especially vulnerable, and so apps and their designers should be mindful of the power they might have in shaping users’ thinking and behaviours. This is particularly important since the world of online mental health support is still a relatively unregulated space. And so Prof. Ilina Singh stresses the importance of taking what we know about what does and doesn’t work well with the face-to-face therapist-patient relationship, and trying to translate this to create online mental health tools (source).
What does the future hold?
Over time we are learning more and more about mental health, including how to treat mental illnesses and how to help patients manage their symptoms. In particular, researchers are interested in finding ways to support young people early on in settings such as school to prevent them from developing mental health problems in the future. Some researchers view digital apps as a potential method to effectively reach out to (some) young people. Alongside this, the media is giving a greater voice to those who face mental health problems through charity campaigns and beyond. This helps to break down the stigma (negative feelings) of mental illness while improving awareness.
That’s not to say that more work isn’t needed… In fact, the (UK) Youth Index, which measures young people's levels of happiness and confidence across various aspects of their lives, is at an all-time low compared to when this information was first collated 10 years ago (source). But in terms of developing our overall understanding and awareness of mental health, active steps are being taken.
Is technology making us sicker or healthier?
Patrick Thomson (School of Geography and the Environment) is using mobile internet technology to prevent people from contracting diseases from dirty water. In sub-saharan Africa, hand pumps are used to collect clean underground water - until the pump breaks. By attaching a small motion sensor - called an accelerometer - to the handle, the pump becomes ‘smart’. It can detect when it’s broken and text a mechanic for help. Thanks to the ‘smart hand pump,’ the communities who have one will no longer need to wait as long for their access to clean water to be restored.
Despite the many benefits, there can also be a human cost to technological advancement. In rural China factories, waste plants and mines have sprung up on the edge of small towns and villages. Through their various activities, many of these sites pollute the air, waterways and soil all around, which has a knock-on effect on any crops grown nearby. Publication of research by academics like Prof. Anna Lora-Wainwright (School of Geography and the Environment) has led the media to dub these areas ‘cancer villages’, due to the higher incidence of cancer among the residents. Although local people are aware of the effect that the pollution is having on their health, economic inequality prevents them from leaving and political pressure means they can do little to challenge the polluters. For now, they have to bear the cost of new technology.
In Uganda, low-cost smart phones and tablets are being utilised in the fight against killer diseases like pneumonia and malaria. The technology enables trainee health workers in remote locations to learn all about diagnosis and treatment by watching videos. Research shows that these health workers remembered the same amount of knowledge after watching the videos than they would if they’d attended training in person (source). Through this kind of digital training thousands can access life-saving information quickly and cheaply and it’s hoped that many more will benefit.
Scared of heights? Spiders? Clowns? New technology is making it possible to face your fears remotely, without needing to bungee off a bridge or hold a tarantula. Daniel Freeman, a professor of clinical psychology, is pioneering the use of virtual reality to treat and understand mental health issues like anxiety and phobias. Participants in a recent fear of heights trial reported that their feelings of fear had been reduced by as much as 68% (source); which is good news for spiders and clowns everywhere!
https://www.youtube.com/watch?v=wC378xuUSp4
Those big adverts on billboards all over the UK were clear... being overweight is bad for your health, just like smoking cigarettes. At least, that’s what a national campaign from the charity, Cancer Research UK told us. But many people criticised the ads, saying that Cancer Research UK were wrong to draw such a clear link between your weight and health and that the campaign was a type of 'fat shaming' (read more)
What everyone does agree on is that to keep generally fit and well, we should take some exercise, get some fresh air, and wear sunscreen so not to burn in the sun and increase our risk of skin cancer.
But if we do all these things, can we avoid disease completely?
Food for thought
Eating plenty of fruit and veggies certainly won’t do any harm to your health -- that’s key to a balanced diet. Dr Marco Springmann of the Oxford Martin Programme on the Future of Food recently helped write a report that says that people across the world eat too much salt, not enough wholegrain (like wholewheat pasta, oats, and brown rice), and definitely not enough fruit (source). This makes us more likely to get sick with things like heart disease or diabetes. Eating less processed and fatty food (takeaways, fry-ups etc.) can go a long way to improving our health.
And, of course, if you can’t steer clear altogether, giving up smoking is a good idea. It helps the health of your heart and lungs and your body starts to repair itself within just a few hours of your last cigarette. Some people think cutting down on cigarettes bit by bit until you’re not smoking any at all is the best way to quit but actually research suggests that stopping all at once is most likely to be successful. A study led by Dr Nicola Lindson-Hawley from Oxford's Nuffield Department of Primary Care Health Sciences says that using things like nicotine patches or gum can help, but picking a day to throw the packs of cigarettes in the nearest bin is the best approach (source). (Of course, if that turns out to be too hard, then cutting down gradually is better than not cutting down at all and just carrying on as you are.)
Small change?
But it’s not as simple as that. Making a change to your lifestyle can actually be very difficult.
Let’s face it, the world is set up to make us less active! For example, about 74% of adults in the UK drive (up from just 48% in the 1970s) (source), and we can order anything we want online rather than leaving our house to look for it. So it’s no wonder that more and more people are heading towards unhealthy lives.
There are also some things that you might think you have complete control over but actually when you’re required to make changes, these changes are really hard to make. For example, what would you do if you were told that you had pre-diabetes (signs of a potentially dangerous health condition that affects how the body deals with eating sugar)? Would you lose weight? Step up a new exercise routine? Research has shown that you’d probably not do very much (source). This is because it’s tough to change the way you behave without lots of help and support from other people, plus some money on top. For example, it can be expensive to get hold of fresh and healthy food and pay for gym memberships or something similar.
Plus, a lot has to do with what types of food we can access. ‘Unhealthy’ food is often cheaper than the 'good' stuff, and simple to get hold of at the nearest takeaway shop. This is particularly true if you can’t travel far because you don’t have your own transport easily available. Therefore, if you’re short of money, it can also mean that you might be more likely to put on weight. In fact, recent statistics show that 17 per cent of fast food shops are in the poorest areas of England with only 3 per cent of them in the richest areas (source).
Money, money, money
So it’s clear that money has a lot to do with how healthy you are. For many years, doctors thought that kids in high-income countries were most likely to have asthma (a breathing condition that can make you cough and wheeze and generally struggle for air). But now, after decades of research, it turns out that children in poorer countries have very high rates of asthma too -- and can have worse symptoms (source).
But why? It could be down to many things. Lack of free, high-quality healthcare, poor air quality, or post-traumatic stress from seeing bad things in the neighbourhood, like violence could all play a role. Stress or feeling sad can make your whole body run differently, including how you breathe. So it’s not just about getting the right medicine when you need it, it’s also about helping kids take care of their mental health and manage their symptoms if they’re suffering from stress, anxiety and/or depression.
Live forever young
The thing is, a lot of the illnesses or problems we face, especially as we get older, are down to our genes -- not just the way we live.
As you get older, you might be more likely to suffer from serious illnesses like heart disease, stroke, dementia, bronchitis and cancer, not because of anything you’ve done, but simply because of the way your body is made up. That said, many people are living longer because of better access to food, good medicine and vaccinations against illnesses that might have killed us a few decades ago. But because we are around for longer, this, in turn, means that we will get more illnesses over the course of our lifespan.
So eat as well as you can, don’t smoke, and take regular exercise; research strongly suggests that this kind of lifestyle reduces your risk of getting sick or frailer as you get older. But sadly, no matter what we do, it doesn’t look like we can end disease completely... not with our current medical and technical understanding anyway. It seems just part of being alive.